Table of Contents
- American Cancer Society Initiative Serves as “BEACON” for Disadvantaged Patients with Cancer Around the World
- Quelling Quarrels: Overcoming Conflict with Colleagues in Oncology Care
- Prehabilitation and Rehabilitation for Patients with Cancer: Focus on Lymphedema
- Vape Pens, e-Cigarettes the Smoking Gun Behind Youth Health Maladies
American Cancer Society Initiative Serves as “BEACON” for Disadvantaged Patients with Cancer Around the World
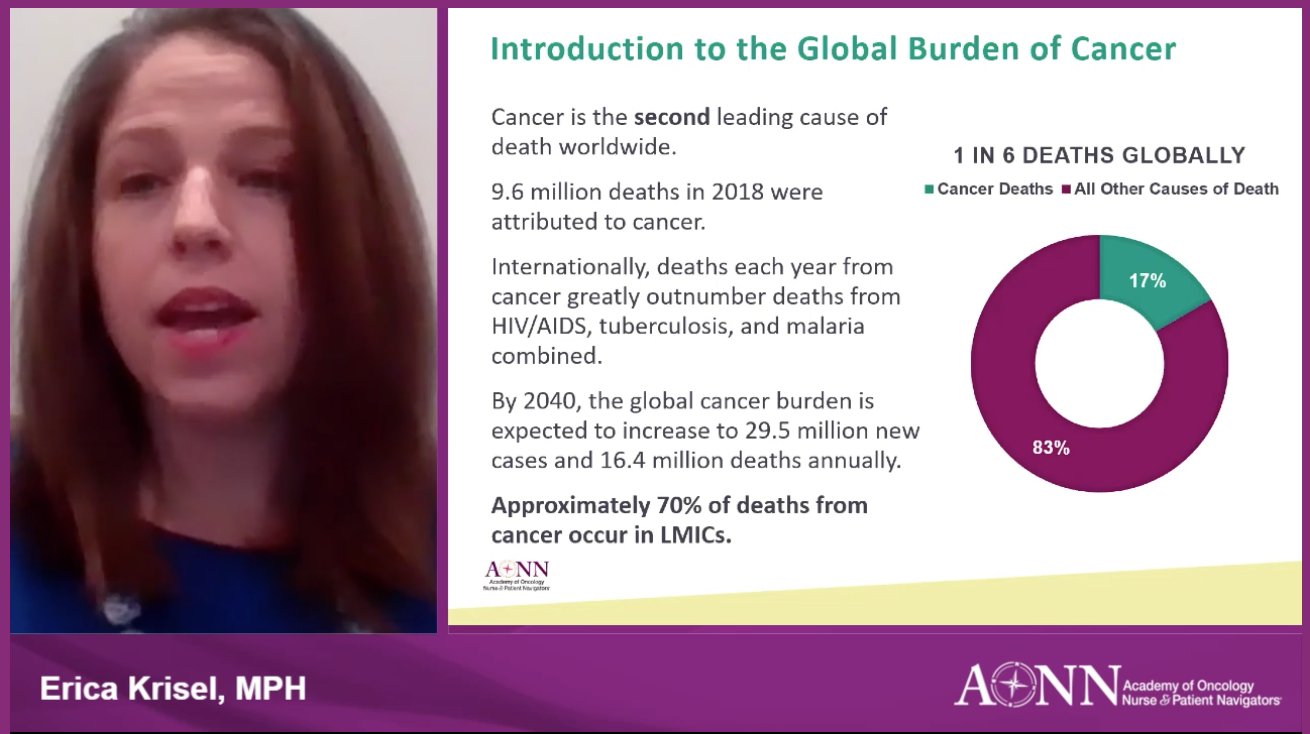
Of worldwide cancer deaths, 70% occur in countries in the low- to middle-income brackets, according to panel members involved in the American Cancer Society Building Expertise, Advocacy, and Capacity for Oncology Navigation (BEACON) initiative. Recognizing the dire need for patient navigation for these populations, members of the BEACON team discussed the development and sustenance of such programs in low- and middle-income countries (LMICs).
“We are making great progress in the US, but that program has not spread to the rest of the world,” said Erica Krisel, MPH.
A 5-year project funded through a grant from the Merck Foundation, BEACON was borne of the rationale that although the magnitude of challenges in LMICs is greater than in the United States and other aspects of cancer care must be addressed, patient navigation—largely unexplored beyond the United States and Canada—has a significant role to play.
With an Advisory Committee whose membership represents 11 countries across 5 continents, including AONN+ members, BEACON is uniquely positioned to address the disparities between high-income countries and LMICs. Although countries with higher income have a greater overall incidence of cancer, their mortality rates are much lower in comparison with LMICs, which show smaller gaps between incidence and mortality.
Helping to combat the disparity is Kenyatta National Hospital (KNH) in Kenya, Africa, where, in 3 years, it has navigated more than 7000 newly diagnosed patients with cancer.
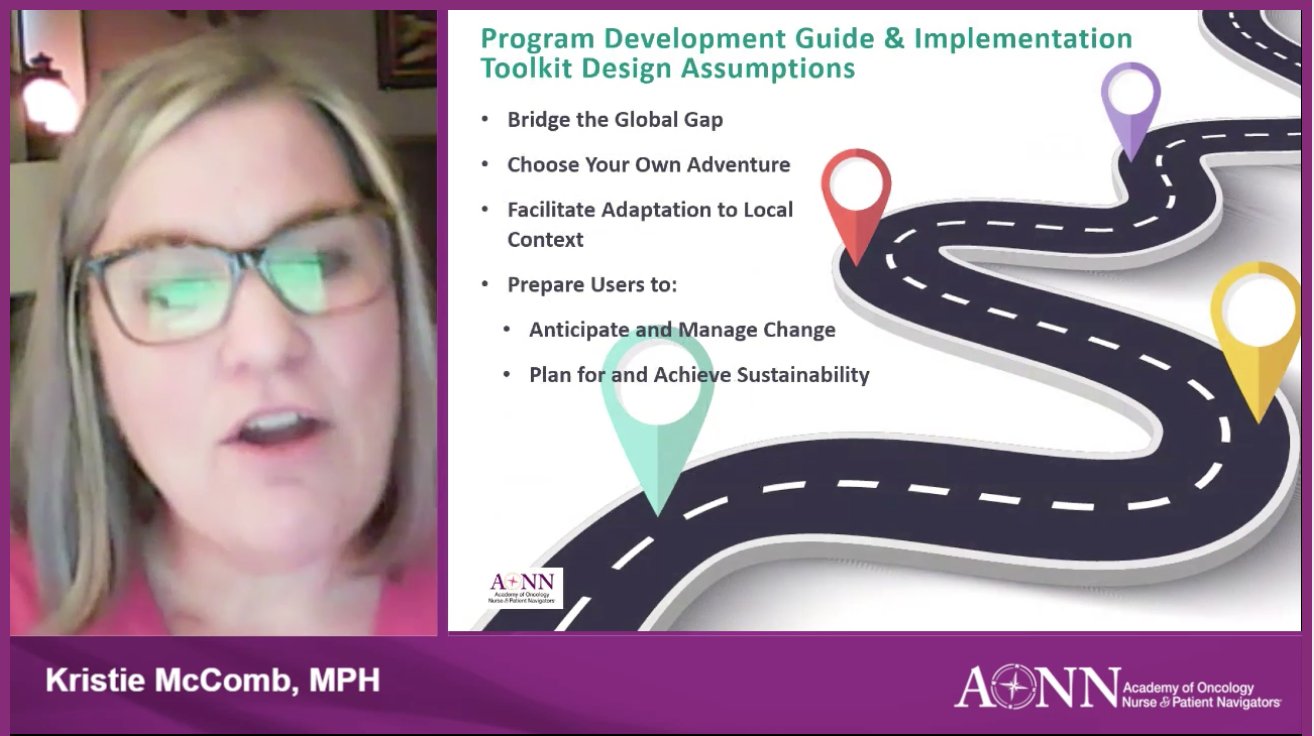
“It is exciting to be doing this work,” Kristie McComb, MPH, said of the opportunity to describe the role of patient navigation throughout the world.
Grace Omulogoli, former patient navigation team co-lead at KNH and American Cancer Society consultant, one of a diverse panel of navigation program leaders from around the world, discussed how the program has enhanced patient knowledge around diagnosis and treatment, as well as helped to ensure patients did not get lost trying to access services.
“This really has shown a great improvement in the experience of our patients in the hospital,” she said.
In Uganda, Africa, Uganda Cancer Institute is set to launch a navigation program in early 2021.
To assist in the establishment of such programs, the creation of a program development guide and implementation toolkit is underway. Seeking to bridge the global gap and facilitate adaptation of navigation programs to local contexts, the guide will prepare users to anticipate and manage change while planning for and achieving sustainability.
“We have also taken a ‘Choose Your Own Adventure’ approach,” Ms McComb said, adding that it was important to remember each country is different and not to impose an Americanized model on budding programs.
These goals will be accomplished with the toolkit’s outlining of phases for program development. In phase 1, program organizers will be invited to create their vision through gaining an understanding of patient navigation and the inner workings of cancer care within their individual health systems, as well as by identifying and engaging their support teams. Phase 2 will consist of the design stage, in which patient navigation will be customized to fit with individual health systems, preparations will be made for implementation and launching of the program, and efforts will be taken to expand the base of support for a program. Implementing and sustaining a navigation program will be the focus of phase 3, which will involve the start of implementation and learning what works; instituting processes and teaching others about them; and measuring progress and communicating successes.
Slated to be a self-guided, self-paced online resource, the toolkit will incorporate video and audio clips, anecdotes from various countries implementing patient navigation, and educational infographics. It will provide valuable support via questions and practical exercises, instructions, templates, worksheets, and curated examples of resources used by other patient navigation programs. Resources will be available for download, and the format of the toolkit will help keep users’ efforts organized and open for refinement over time. Interactive and fun, the toolkit will be bolstered by a Project ECHO® clinic, in which users can share and reflect on their experiences, encourage one another, exchange resources, and work together on problem-solving.
The toolkit is expected to be ready for widespread dissemination by 2022.
Quelling Quarrels: Overcoming Conflict with Colleagues in Oncology Care

Representing a significant source of stress in any workplace, conflict can be particularly troublesome in the oncology field, where pressures already run high. It is important to remember, however, that conflict is natural, inevitable, and if handled well, can be constructive for those involved, according to Helen Meldrum, MEd, EdD, who discussed disputes among colleagues and how best to defuse such situations.
“We need skills to keep things from escalating,” Dr Meldrum said.
Citing surveys of employees in various workplace environments, Dr Meldrum said 64% of workers reported experiencing a toxic personality in their current place of employment, and 94% stated they had worked with such an individual at some point in their careers. In a hospital setting, 91% of nurses reported having experienced verbal abuse. When one considers such statistics, paired with the knowledge that negative interactions affect mood 5 times more strongly than positive ones, it becomes no wonder that workplace conflicts exist.
“I think we’ve all felt the effect of backstabbing, not feeling safe, not feeling we have the ability to speak up,” Dr Meldrum said.
Although conflict in the workplace is unavoidable, the ways in which it is handled make all the difference in determining the outcome. Unconscious patterns can contribute to interpersonal issues, according to Dr Meldrum.
“Without taking the time to think about it consciously, we often create undesirable repetitive patterns,” she said.
For example, a vicious cycle can emerge from those who apply pressure in an effort for their ideas and opinions to be accepted. The pushing can result in others feeling threatened and putting up an internal wall against the ideas and opinions. The resistant individuals may then withdraw into an unresponsive state, which results in the pressuring party applying more of the same to break through that resistance. Another cyclical pattern stems from those who are not good at delegating tasks, because they believe others do not have the energy, drive, or commitment to match their own. Therefore, without realizing it, such individuals communicate mistrust of others’ work ethics, resulting in the others feeling undervalued, mistrusted, and unappreciated. These others often respond by withholding their energy, commitment, and full potential, bringing the ineffective process full circle.
Adding to these dynamics is that oncology clinicians can often feel uncomfortable, edgy, and embarrassed, thereby possibly coming across to others as cold, insensitive, and brutal, Dr Meldrum said. Compassion fatigue and burnout also contribute to conflict, she added.
Traits among healthcare providers can be determinants of success or failure, also determining how they will fare in relationships with their colleagues. A clinician can be equipped for success by:
- Having a positive attitude
- Staying focused on the patient
- Maintaining high energy
- Embracing challenge and remaining flexible
- Allowing others to be right.
Conversely, setting oneself up to flounder or fail involves:
- Being depressed and feeling angry or stuck in a job
- Needing a lot of attention
- Being overly laid back
- Needing order and predictability
- Having to always be right.
Just as personalities differ, each person has their own style when it comes to contending with conflict. These consist of avoidance, accommodation, competition, compromise, and collaboration. Whatever one’s style, skills are necessary to defuse conflicts before they have a chance to escalate. These involve reflection, deflection, inquiry, feedback, and deferral.
Active, reflective listening is a key component of effective communication that involves determining whether the speaker is mad, sad, glad, scared, or any other mix of emotions. Such listening moves away from a reactive stance and into one of understanding. Active listening never involves judging, advising, quizzing, or placating the speaker, Dr Meldrum said.
An empathic, reflective response is one that helps to create a feeling of alignment with an individual, showing understanding and genuine care.
“Match it and they tell you more; miss it with the judging, advising, quizzing, and placating, and you’ll never find out,” she said.
Deferral is an important skill to master, necessary in situations where one may be in danger.
“You’re always going to want to have a line ready if they’re more than angry and clinical symptoms are present,” Dr Meldrum advised.
In dealing with workplace conflicts, a mnemonic device can prove helpful when in the midst of a heated moment. Dr Meldrum shared with attendees the following acronym:
- C – Clearly describe the issue
- L – Listen, using the active listening techniques described
- E – Express emotion
- A – Assert your opinion in a clear, calm manner
- R – Communicate the results expected in a positive way.
Prehabilitation and Rehabilitation for Patients with Cancer: Focus on Lymphedema
With goals of maximizing function and improving quality of life, rehabilitation is a key component of cancer care. Cancer and its treatment impact function in patients, with functional loss occurring in a slow, gradual manner that is difficult to detect in its early stages. Asserting that physical function should be treated as a vital sign in patients with cancer, Adrian Cristian, MD, and Joy C. Cohn, PT, discussed the importance of rehabilitation medicine, including prehabilitation, with a focus on managing lymphedema.
Different cancers and their treatments are accompanied by varied impairments, which share the common ground of impeding function and often affecting patients’ ability to work. Although 63.5% of cancer survivors return to work, patients with cancer miss an average of 151 workdays and 26% to 53% of cancer survivors lose their jobs or stop working over a 72-month period after diagnosis. Affecting patients’ ability to work are physical symptoms, poor sleep, daytime fatigue, and decreased job performance.
“That’s where rehabilitation medicine can improve an individual’s ability to return to work,” Dr Cristian said.
Occurring between a cancer diagnosis and the start of treatment, prehabilitation is aimed at reducing the incidence and severity of future impairments and promoting physical and psychological health. It involves establishing patients’ baseline functional level, as well as identifying and treating impairments through nutritional counseling, anxiety reduction, smoking cessation, and exercise.
“Early intervention is key,” Dr Cristian said.
Barriers to rehabilitation include lack of patient and caregiver education about cancer-specific impairments and rehabilitative interventions, along with geographic and insurance-related issues. For some patients, childcare, work obligations, and other life demands get in the way of receiving necessary rehabilitation. Navigators, however, can help topple these barriers through early identification of impairments and by advocating for patients to receive this care, according to Dr Cristian.
As cancer-related impairments vary by cancer site, identification of these impairments varies accordingly. The presenters offered recommendations on areas to examine in patients, depending on their cancer type. For head and neck cancers, navigators should focus on swallowing, opening the mouth, neck swelling, and shoulder problems, along with weight loss. For breast cancer, the focus should be on shoulder pain and restriction of movement, arm swelling, hand pain, nerve-related symptoms, memory loss, spine pain, and weight gain. Gastrointestinal, genitourinary, and gynecologic cancer call for identification of incontinence, sexual dysfunction, leg swelling, nerve pain, impaired balance, and weakness and decreased use of hands. For lung cancer, shortness of breath, nerve pain, balance issues, spine pain, and memory loss are significant issues. In brain and spine cancer, navigators should watch for weakness in limbs, balance issues, memory loss, impaired attention, and incontinence. Hematologic malignancies should be monitored for spine and nerve pain. In all cases, the impact of symptoms on work and social roles should be evaluated, the presenters advised.
In determining whom to refer for rehabilitation, navigators should identify those who cannot raise their arm overhead, stand on one leg for 10 seconds, or get up out of a chair 10 times in 30 seconds. Others to refer include patients who would benefit from a clinical trial but are considered too frail to participate, and all patients with stage IV cancer.
Lymphedema
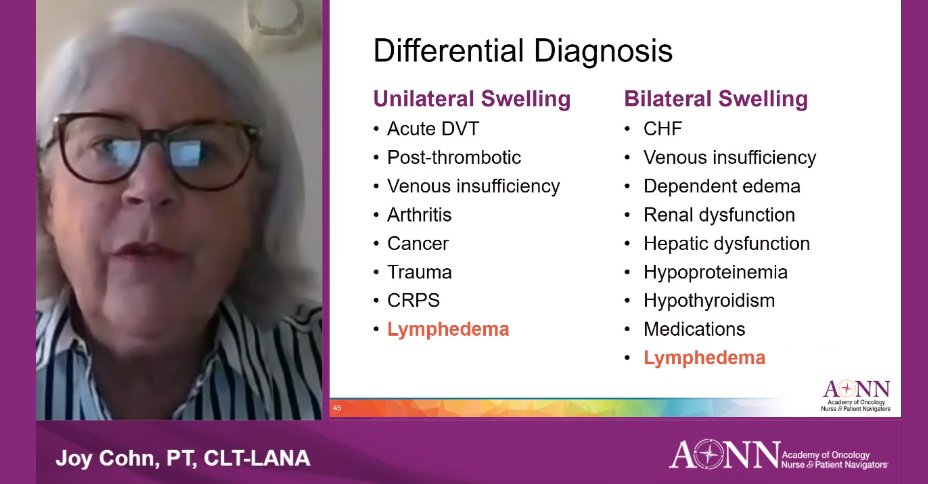
Playing an important role in overall health, the lymphatic system recycles proteins, drains the interstitial space, conducts immune surveillance, and transports digested fats. Often caused by cancer and its treatment, secondary lymphedema has the greatest incidence in patients with head and neck cancers, reaching 75%, although it can occur in cancers of any type. Risk factors include nodal dissections, radiation to nodal regions, obesity, extensive surgeries, and preexisting venous disease in lower extremities.
“Differential diagnosis is really a key for me when a patient comes in with edema,” Ms Cohn said. “Lymphedema is only one of many things it could be.”
Occurring in 4 stages, lymphedema comes with symptoms that include numbness, tightness, stiffness, pain consisting of aching or heaviness, infection, redness, heat, and the signature swelling. Malignant lymphedema can be the first sign of cancer recurrence, and is characterized by rapid onset, significant edema, among other signs. In such cases, clinicians must ask for input from the oncology team before treatment.
“This may represent a recurrence,” she advised, adding, “The gold standard here in the United States is complete decongestive therapy.”
This consists of manual lymphatic drainage, multilayer compression bandaging, exercise, and meticulous skin care in the intensive phase, along with garment wear, compression at night, and exercise in the maintenance phase.
Vape Pens, e-Cigarettes the Smoking Gun Behind Youth Health Maladies
Although cigarette smoking has shown a marked decline in the United States in recent years, vaping has stepped in like a slick charlatan, wooing young people into an equally deadly habit. Educating navigators on electronic nicotine delivery systems (ENDS) and their dangers, Nancy Sayegh-Rooney, RN, ONN-CG, NCTTP, a lung nurse navigator, also shared information about prevention efforts and clinical implications of vaping.
“These products are not taxed, nobody knows what’s in them, and they don’t have to answer to any regulation,” Ms Sayegh-Rooney said. “It’s really scary stuff.”
When one considers that nearly all tobacco use begins during adolescence, it makes sense that ENDS are offered in a variety of enticing flavors that could seduce young tastes. Seemingly innocuous to young people, these palatable puffs represent a wolf in sheep’s clothing, Ms Sayegh-Rooney said. Thanks to targeted marketing, a 48% increase in vaping has been seen among middle school–aged children, and the Centers for Disease Control and Prevention (CDC) reports that the use of e-cigarettes increased by up to 78% among high school students between 2017 and 2018. In 2018, 27.1% of high school students reported use of any tobacco product. Of them, 20.8% used e-cigarettes.
The most popular among e-cigarettes, 1 Juul is equivalent to 3 packs of cigarettes, according to Ms Sayegh-Rooney.
“We’ve got an issue,” she said. “We’ve stopped talking, but we’ve got to continue the conversation with these kids. We need to explain to them, without our breath, we are nothing.”
While some may view vaping as relatively harmless because of the lack of foul-smelling smoke, this could not be further from the truth. Like traditional cigarettes, e-cigarettes contain nicotine, which is not only highly addictive but also can harm the developing brain, impairing learning, memory, and attention, according to Ms Sayegh-Rooney.
“It is a gateway drug to a lifetime of nicotine dependency. We’ve created a new generation of addicts,” she said.
Nicotine is not the only danger lurking inside ENDS, which include e-cigarettes and “pods.” The vapors being inhaled from these devices also contain glycerol, a colorless, sweet, viscous liquid. Formed as a byproduct of soap manufacturing, glycerol is used as an emollient and a laxative, and is also used for making explosives and antifreeze. Propylene glycol, a carcinogenic byproduct of fossil fuel, is often used to create polyurethane plastic, and is used in ENDS. Other unsavory ingredients include benzoic acid, a chemical used in insect repellent, and vitamin E acetate, a thickening agent often used in THC vaping products. Despite their toxic makeup, ENDS are only predicted to grow in popularity.
Advocacy efforts to quell the craze are underway, and seek to target the underlying drivers of vaping. So as not to reinvent the wheel, advocates are working on modernizing evidence-based tobacco-control strategies that have worked in the past. These include price increases, indoor-use restrictions, and educational campaigns, along with flavor restrictions to make ENDS less attractive to young people, said Ms Sayegh-Rooney.
“We all share an important responsibility to keep these harmful and addictive products out of the hands of our kids,” she added.
From a clinical standpoint, vaping raises considerable concerns. Most recent among them is the significantly increased risk for COVID-19 among teens and young adults who vape, according to a study conducted at Stanford University School of Medicine. The researchers found that among participants tested for COVID-19, those who had ever used e-cigarettes were 5 times more likely to be diagnosed with COVID-19 than nonusers. In addition, young people who had used cigarettes or e-cigarettes in the past 30 days were nearly 5 times as likely to experience symptoms of COVID-19, including coughing, fever, fatigue, and breathing difficulties, as those who never smoked or vaped.
Combine this added risk with the risk for “popcorn lung” or bronchiolitis obliterans, along with e-cigarette or vaping product lung injury (EVALI), and it becomes clear that vaping is a recipe for disaster. As of January 2020, 2602 cases of EVALI were reported to the CDC; 57 of those cases resulted in death.
Diagnosing EVALI can be a challenge, as symptoms mimic those of other respiratory illnesses, Ms Sayegh-Rooney advised.
“It’s similar to the illnesses of pneumonia and the flu,” she said. “It’s similar to what we see on a COVID x-ray.”
Treatment involves corticosteroids, antibiotics, and antivirals, she said, pointing out that follow-up is vital because data are pending on long-term effects.
“We don’t know how long their recovery will be. We don’t know what the long-term effect will be from this…diagnosis,” Ms Sayegh-Rooney said. “It’s really a scary time that these products are out there and our children, our grandchildren have access to them.”














