Table of Contents
- Preconference Workshops Allow for Additional Learning Opportunities
- AONN+ Awards Recognize Excellence in Navigation
- Telehealth and Oncology Navigation: Delivering Care Digitally Amid the Pandemic
- The AONN+ Navigation Metrics Toolkit: Equipping Programs to Measure Success
- Vicarious Trauma: When Patient Pain Hurts the Provider, Too
- When the Clock Is Ticking: The Importance of Fertility Preservation for Adolescent and Young Adult Patients with Cancer
Preconference Workshops Allow for Additional Learning Opportunities
Attendees seeking to be at the forefront of knowledge in navigation field got a jump on annual conference proceedings by virtually attending 4 preconference workshops that addressed issues of importance to navigators.
Genetics and Genomics

Key to providing personalized medicine in cancer care, genetic and genomic testing and the issues surrounding them are areas of knowledge with which navigators must be equipped. Frank dela Rama, RN, MS, AOCNS, AGN-BC, and Jennifer Klemp, PhD, MPH, MA, who together co-chair the AONN+ Genetics and Genomics Committee, along with other experts, provided the opportunity to gain such knowledge during their workshop on the topic.
“The current state of genetics and genomics is really so fluid,” Dr Klemp said. “There’s nothing static about it.”
In line with the Building Relationships in Delivering Genetic/Genomic Education (BRIDGE) program, whose goal is to use educational interventions to best connect oncology nurse and patient navigators to cancer genetics and genomics professionals, the BRIDGE symposium sought to arm navigators with the tools to educate patients and advocate for appropriate referrals to genetic professionals, ensuring access to appropriate testing.
“It’s everybody’s responsibility to make sure we’re referring the patients appropriately,” said Elisabeth King, RN, FNP, AOCNP, AGN, adding, “Know the red flags for hereditary cancer syndromes. [National Comprehensive Cancer Network guidelines] are your friend. You don’t have to know everything. Let’s do this together.”
Financial Navigation
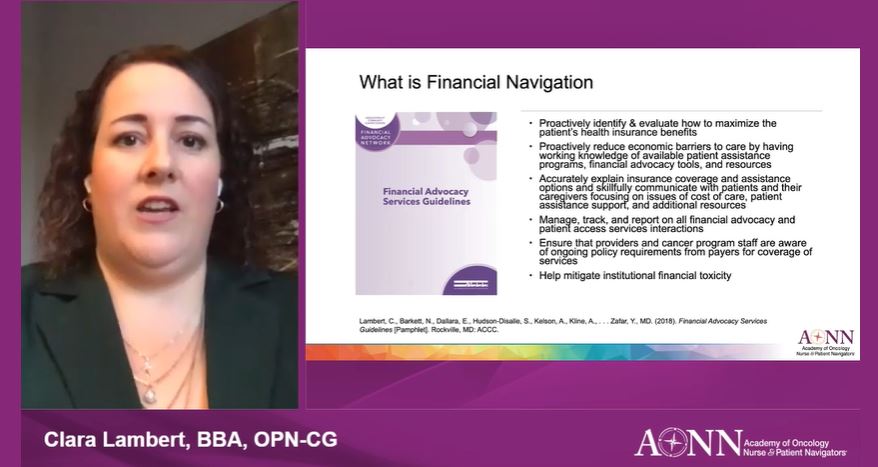
Among the myriad changes the COVID-19 pandemic has sprung upon the world, financial difficulties represent one of the most impactful. Oncology navigators are already aware of the importance of financial navigation within a cancer program, and the new economic landscape has only enhanced the critical nature of these services, which involve helping patients through the process of determining how to pay for their care, through insurance coverage and/or financial assistance.
“It’s really important to prepare for the patient,” said Angie Santiago, AA, CRCS. “From the patient perspective, it really shows we’re there to support them.”
This workshop provided a primer on how navigators can show the worth of their current financial navigation programs or gain administrative buy-in to start a new one; evaluate pre-emptive screening for financial toxicity and build community support for those facing it; and construct a strong foundation for financial navigation programs using frameworks provided by national experts in the field. In addition, the presenters discussed resources for financial navigation programs, including new financial technology tools, as well as how to measure and track such programs to demonstrate their success.
“Track, track, and track some more,” advised Nikki Barkett, BSN, RN, OCN, saying it helps to provide evidence of the value of financial navigation programs.
Professional Development

A collaborative effort among the experts on the AONN+ Leadership Council, the professional development workshop incorporated the varied voices of leaders in the field to offer insights on team-building, coaching, and how to meet challenges that arise for those in leadership roles.
“Navigators must commit to lifelong learning and the pursuit of continuing education,” said Cheryl Bellomo, MSN, RN, OCN, HON-ONN-CG. “Staying current in navigation practice is a key component of professional development.”
Participants also gained knowledge on individual leadership styles, along with methodologies to collaborate, communicate, and interact with fellow professional leaders.
“I think we’re always figuring out new ways to be leaders,” said Jennifer Bires, MSW, LICSW, OSW-C, adding that shared goals comprise an important component of this. “We always want to build buy-in with our team members, and one way of doing this is making sure everyone has a stake.”
Motivational Interviewing
Providing national leadership for the development, education, standardization, and sustainability of patient navigation, the Patient Navigator Training Collaborative offered a piece of the exclusive curriculum they regularly offer to navigators through their program. Andi Dwyer, BS, Patricia Valverde, PhD, MPH, and Erin Martinez, MPH, outlined techniques for motivational interviewing, a counseling style rooted in social work that helps to elicit positive behavioral changes in patients.
“It’s about the client, Dr Valverde said. “It’s all focused on enhancing the person’s own motivation to change.”
AONN+ Awards Recognize Excellence in Navigation
Touching on various areas of the care continuum, the AONN+ awards are a highlight of the annual conference, with navigators stepping up as unsung heroes to be honored for their valuable contributions. This year was no exception, with the usual celebratory tone intact despite the inability to meet face-to-face.

Perhaps most moving among the honors was the CONQUER: the patient voice Hero of Hope Award, which recognizes an oncology patient for outstanding contributions to the cancer community. Khadijat Fatai-Banwo, a 10-year survivor of HER2 triple-positive breast cancer and patient advocate in Nigeria, could not have been more perfectly suited for the award. Having lost her husband 7 days after a radical single mastectomy, Ms Fatai-Banwo did not allow her cancer battle or profound loss to stop her from enacting positive change.
Ms Fatai-Banwo co-founded Project PINK BLUE (PPB), a nonprofit aimed at raising cancer awareness, as well as providing patient navigation, advocacy, and free breast and cervical cancer screenings for women in poverty. The organization has reached more than 25 million people. The breast navigator at PPB, Ms Fatai-Banwo’s passion, is to change the cancer paradigm in Africa. Also co-founder of the Abuja Breast Cancer Support Group, she was instrumental in developing the Breast Cancer Navigation and Palliative Program at PPB with a grant from Union for International Cancer Control. A certified patient navigator at George Washington Cancer Center in the United States, Ms Fatai-Banwo is a champion for gender equality and other gender-related issues.
“Wow, what she has done is totally incredible,” AONN+ Program Director Sharon Gentry, MSN, RN, HON-ONN-CG, AOCN, CBCN, said of Ms Fatai-Banwo.

Named for AONN+ Co-Founder and retired Program Director, the Lillie D. Shockney Lifetime Achievement Award recognizes a member who has made remarkable contributions to oncology navigation, as well as to AONN+. Awardee Danelle Johnston, MSN, RN, HON-ONN-CG, OCN, who has served as a trailblazing leader for the organization over the past 3 years, initiated and nurtured partnerships with numerous oncology organizations, and offered invaluable clinical and professional insights that have helped AONN+ to thrive. Her vision gave birth to the processes, policies, procedures, and role descriptions that have given AONN+ its structure. An adept leader, Ms Johnston’s tireless efforts and countless initiatives have helped to make AONN+ what it is today.
“It is with professional pride but also personal pride that we have chosen Danelle to receive the Lillie D. Shockney Lifetime Achievement Award,” Ms Shockney said.

In recognition of its patient navigation program, Sarah Cannon received the AONN+ Organization Award. Based in Nashville, TN, Sarah Cannon encompasses multiple cancer centers nationwide, as well as one in London, UK, with a formalized process at these centers allowing nurse navigators to comprehensively manage a patient’s experience with cancer.
Bestowing special honors on the leaders of these efforts, Michelle Rowe, RN, BHCA, Assistant Vice President of Clinical Operations; Brook Blackmore, RN, MBA, MSN, Senior Director of Navigation Operations; and Judy Koutlas, RN, MS, OCN, Senior Director of Navigation Operations, AONN+ leaders called out their commitment to professional development and lifelong learning.

An exceptional leader, Elizabeth Franklin, PhD, MSW, Executive Director of the Cancer Policy Institute at the Cancer Support Community, Washington, DC, was aptly chosen to receive the AONN+ Ambassador Award. As leader of the AONN+ Policy and Advocacy Committee, Dr Franklin used her experience and diplomacy to help make the Academy part of the national healthcare discussion. Providing valuable contributions during her service on the AONN+ Leadership Council, she offered knowledge and insights to promote inclusivity and multidisciplinary approaches to navigation.
The Central Indiana Local Navigator Network (LNN) received the Outstanding LNN Award in recognition of its exceptional work in establishing an open forum for professional development and networking that aligns with the AONN+ mission.

The Putting Evidence into Practice Award honors an AONN+ member who has conducted evidence-based research that supports navigation. Having served on the AONN+ Leadership Council, Jennifer Klemp, PhD, MPH, Associate Professor of Medicine, Division of Clinical Oncology, Director of Cancer Survivorship, and Co-Program Leader for Cancer Prevention and Survivorship at the University of Kansas Cancer Center, is Co-Chair of the Genetics and Genomics Committee. In that role, she contributed to the Building Relationships in Delivering Genetic/Genomic Education (BRIDGE) program, which seeks to give all navigators a working knowledge of genetics and genomics, so that they may better advocate for patients.
Telehealth and Oncology Navigation: Delivering Care Digitally Amid the Pandemic
Telehealth has seen a significant surge since the first US COVID-19 shutdowns in March, with state and federal regulatory changes allowing for the necessary expansion of virtual visits. Remote provision of healthcare has only expanded since then, allowing for oncology navigators to incorporate telehealth into their robust repertoire, according to Jennie R. Crews, MD, MMM, and Janelle Wagner, RN, OCN, who discussed telehealth legislation, opportunities, and challenges in this relatively uncharted landscape.
“Historically, there has not been widespread adoption of telehealth, particularly in oncology,” Dr Crews said, adding, “And then along came COVID this winter and we had to quickly change our response.”
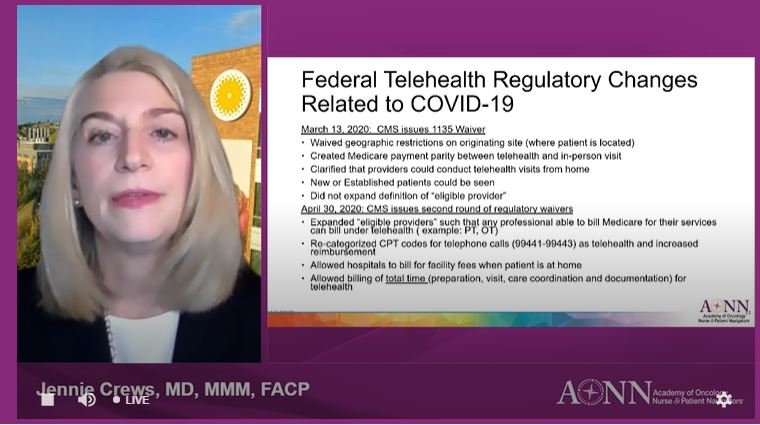
In response to the declaration of COVID-19 as a pandemic by the World Health Organization and as a national emergency by the President, the Centers for Medicare & Medicaid Services (CMS) issued an 1135 waiver, which loosened restrictions on telehealth services and created Medicare payment parity between telehealth and in-person visits. By the end of April, CMS issued a second round of regulatory waivers, allowing for all types of healthcare providers to bill Medicare for telehealth services, along with other provisions. Some of these provisions, however, will not continue into the 2021 Physician Fee Schedule, the presenters explained.
Federal and state legislation have also moved to expand telehealth access and coverage. If passed, a proposed telehealth “superbill” would further ease the widespread use of telehealth, including the establishment of a national telehealth program, as well as federal studies on the expansion of telehealth access under Medicare and Medicaid.
Although it’s clear telehealth has a strong foothold, the presenters predicted regulatory changes when the emergency declaration is lifted, with state licensure requirements likely returning to their pre–COVID-19 status. Strong advocacy efforts are in place, however, to maintain the patient’s home as an acceptable originating site, payment parity or equity, and the wide array of providers currently allowed. In addition, efforts are underway to enhance patient access to telehealth through the provision of broadband and/or devices where the need exists.
“It has opened a whole new world for us, and I don’t see that going back,” Dr Crews said.
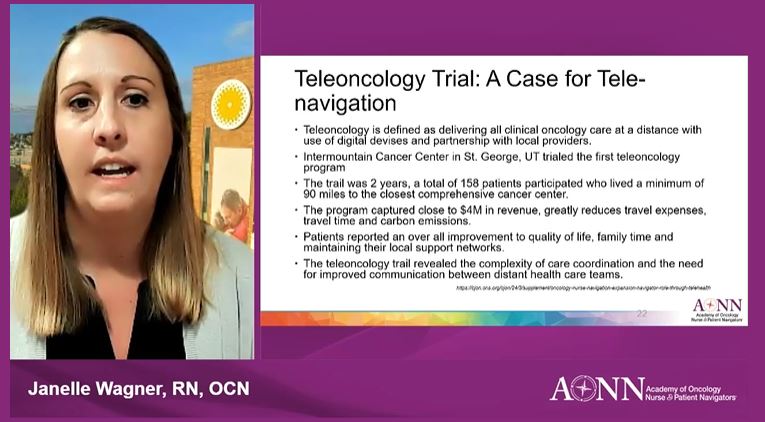
The presenters cited a 2-year tele-oncology trial at Intermountain Cancer Center in St. George, UT, as the first of its kind. Enrolling 158 patients who lived a minimum of 90 miles to the closest comprehensive cancer center, the program captured nearly $4 million in revenue while significantly reducing travel time and associated expenses, along with carbon emissions. Participants reported overall improvements in quality of life and other measures. The trial revealed the complexity of care coordination and the need for improved communication between distant healthcare teams.
A key component to tele-oncology, telenavigation is care coordinated by an oncology nurse navigator in tandem with the care team, patient, and family, using technology. Although the literature on tele-oncology highlights the importance of telenavigation, few data are available on its benefits, the presenters explained, adding that institutions should incorporate telenavigation and track its benefits to optimize this care modality for patients.
“With all the new laws that support telehealth, it’s just the time to bring this to your institution,” Ms Wagner said.
The AONN+ Navigation Metrics Toolkit: Equipping Programs to Measure Success
Although those most familiar with navigation would never doubt its value, the current climate of value-driven healthcare demands the demonstration of quality and outcomes. Recognizing this, AONN+ leaders undertook the task of creating, researching, and guiding the implementation of evidence-based navigation metrics.
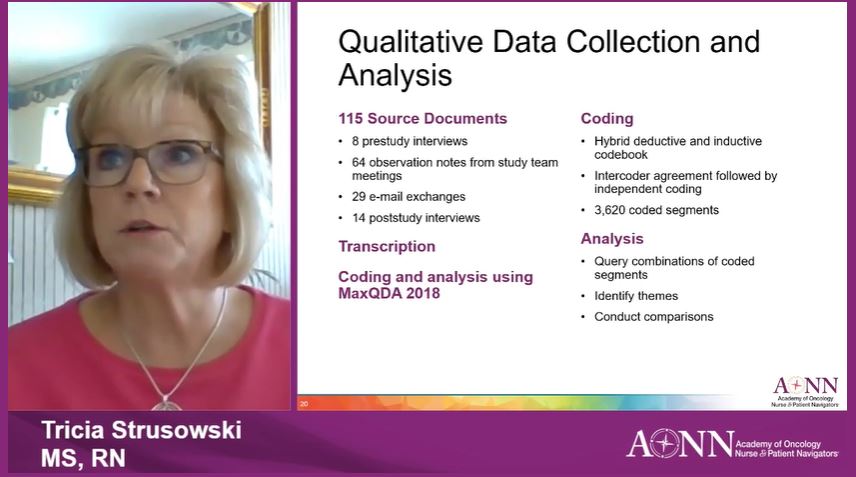
“We believe the navigation metrics will really be transformative to cancer care,” said Monica Dean, HON-OPN-CG, AONN+ Director of Patient Navigation Program Development, who led the session alongside Danelle Johnston, MSN, RN, HON-ONN-CG, OCN, and Tricia Strusowski, MS, RN.
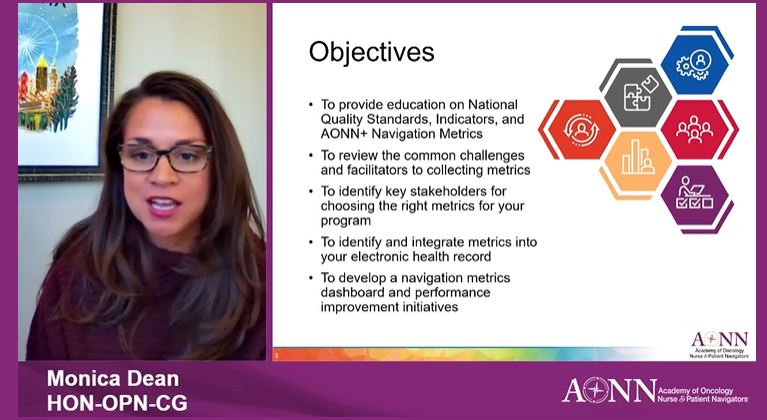
In 2017, AONN+ identified 35 evidence-based navigation metrics that were most relevant to oncology care, based on patient experience, clinical outcomes, and return on investment. The following year, the Academy partnered with the American Cancer Society and Chartis Oncology Solutions to conduct a multisite national research study on the metrics in action. The efforts have culminated in 2020 with the completion of the AONN+ Navigation Metrics Toolkit, which is aimed at helping navigators, oncology program administrators, healthcare executives, and other clinicians involved in navigation to understand, support, and implement the integration of standardized metrics into their normal business processes.
“This toolkit has been a labor of love for all of us and we’re just so excited to share this with you,” Ms Dean said. “I think the toolkit is going to provide some great guidance and great examples for navigation programs.”
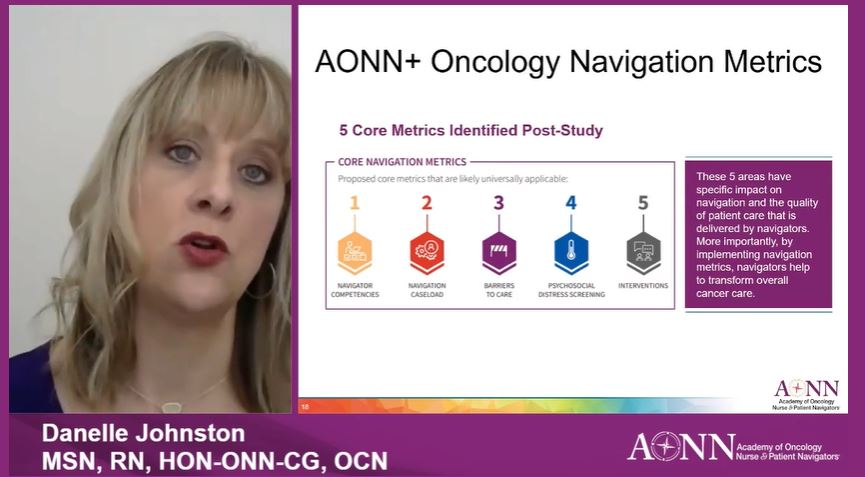
Of the 35 metrics first identified, members of the Metrics Committee chose 10 to include in the research study. After reviewing the study results, these were whittled down to 5 core metrics found to have the greatest impact on oncology navigation and deemed likely to be universally applicable. These are:
- Navigator competencies
- Navigation caseload
- Barriers to care
- Psychosocial distress screening
- Interventions.
“They’re baseline metrics that all institutions can use, regardless of the model of navigation,” Ms Johnston said.
Collecting metrics data can seem like yet another burden on the shoulders of navigators, but in reality, the demonstration of value is an overall asset to navigation programs.
“This is part of our role as navigators, and it needs to be reflected in our job descriptions and role delineations,” Ms Strusowski said. “You are in a very unique position in the healthcare team to help do healthcare transformation and that’s why metrics are so important, because they help you tell your story.”
Limitations to qualitative data collection pose an issue. Because data primarily come from site leads and navigators, they can overemphasize the navigator’s perspective, without taking into account other relevant perspectives. As a result, findings may underestimate barriers for metrics data that are not collected directly by navigators. In addition, variations in responses can create bias, as sites differed in their willingness to provide candid feedback. With this in mind, the analysis focused on facilitators and barriers to data collection identified at multiple sites, instead of making cross-site comparisons, according to Ms Strusowski.
Facilitators to data collection include aligning the process with existing workflows, creating a unified template to capture metrics, using discrete reporting fields, and gathering support from IT, clerical/administrative teams, and the study team, she said.
Perhaps most important to demonstrating value through metrics is garnering the support of key stakeholders within an institution or health system. Finding a physician champion to support the metrics measurement process is a great first step, as is eliciting buy-in from others in leadership positions, Ms Johnston said. Other key stakeholders with whom to seek engagement include IT directors and electronic health record providers, social workers, health psychologists, tumor registry representatives, case managers, clinical trial representatives, performance improvement/quality representatives, patient/family caregivers, and billing staff. Navigators can work with these stakeholders to determine which metrics are best for their programs. It is best to include metrics that fit with existing program goals, as well as ones that incorporate data being collected or reported elsewhere.
“When these metrics aligned with preexisting workflows, it was much more natural for the navigators,” Ms Strusowski said.
As data are gleaned and analyzed, it is important to compile it in a simple, digestible format. That is where the navigation metrics dashboard comes in, Ms Strusowski said. By creating a dashboard, programs can convey data so it can easily be shared with program directors and administrators.
For further information on the AONN+ navigation metrics, visit aonnonline.org/navigation-metrics. The AONN+ Navigation Metrics Toolkit can be found at aonnonline.org/images/resources/navigation_tools/2020-AONN-Navigation-Metrics-Toolkit.pdf.
Vicarious Trauma: When Patient Pain Hurts the Provider, Too
Empathy and caring are prevalent among those in the helping professions, and navigators are no exception. Although these characteristics are central to helping others, they can also become a detriment by causing the healthcare provider to internalize patients’ suffering—a phenomenon known as “vicarious trauma,” according to Bina Parekh, PhD, the keynote speaker at the AONN+ Virtual Annual Conference.
“Vicarious trauma is a cumulative experience,” she said. “A lot of times, people don’t even recognize that they’re experiencing vicarious trauma.”
With an emphasis on the COVID-19 pandemic and the trauma it has wrought for so many, along with the civil unrest that has been taking place throughout the country in recent months, Dr Parekh pointed out a common thread. Patients with COVID-19 have had diminished breathing capacity, and the haunting refrain of George Floyd as he lay dying under the knee of a police officer was, “I can’t breathe.”
“We have to take a moment to breathe,” she told attendees.
Resulting from engaging with people and their traumas in an empathic way, vicarious trauma can lead to compassion fatigue and burnout. Not unique to healthcare providers, it also affects therapists and counselors, clergy, first responders, and others who provide care to distressed individuals.
“I think this is very much heightened with COVID-19,” Dr Parekh said.
As evidence, she shared a video of a nurse who worked on a COVID-19 unit at a hospital. The nurse tearfully recounted her experiences and expressed feelings of despair and powerlessness. Those caring for individuals with COVID-19 are often hit hard by vicarious trauma in addition to the traumas endured directly amid the pandemic, in the healthcare setting or elsewhere, Dr Parekh explained.
The ongoing pandemic has created a unique situation of collective trauma, which is a traumatic psychological effect shared by a group of people.
“All of this is impacting the entire fabric of society concurrently,” Dr Parekh explained, adding that half of 9/11 first responders reported symptoms of posttraumatic stress disorder 11 to 13 years later.
Often as impactful as firsthand trauma, vicarious trauma can cause symptoms, including:
- Feelings of self-loathing
- Hopelessness
- Negative outlook
- Emotional numbness
- Feeling overwhelmed
- Withdrawal from friends and family
- Intense rage or crying bouts
- Despair
- Exhaustion
- Anxiety
- Nightmares
- Resentment
- Feeling unsafe.
More than simply a constellation of symptoms, vicarious trauma affects one’s whole being, having a marked impact on a person’s sense of self, according to Dr Parekh. Its effects often extend to the provider’s identity, world view, spirit, cognition, and ability to provide self-care.
“Their worldview shifts from a place of trust to a place of fear, mistrust, and cynicism,” she said. “It erodes the faith and meaning in our work.”
Although anyone can experience vicarious trauma, certain factors place an individual at higher risk. Personal factors include having a history of trauma or a preexisting psychological disorder, young age, inadequate support system, having suffered a loss within the previous year, or possessing particular personality traits. Professional risk factors for vicarious trauma are a lack of job orientation, training, quality supervision, or experience. Other professional risk factors include a patient caseload that includes a high percentage of trauma survivors and a mismatch between a worker and an organization, she said.
When one considers that more than 60% of men and more than 50% of women have experienced 1 or more traumatic events and that 90% of clients in public healthcare settings have undergone trauma, it becomes no wonder that between 40% and 80% of helping professionals develop vicarious trauma, compassion fatigue, or traumatic symptoms, Dr Parekh said.
Acknowledging the potential harm caused by vicarious trauma, assessments seek to measure its impact on healthcare providers and others. These include the Professional Quality of Life Scale, Secondary Trauma Stress Scale, and Maslach Burnout Inventory.
Fortunately, in the same way patient trauma can have a vicarious effect, their resilience can also have an impact on those caring for them. As patients move toward adapting to and even overcoming adversity, navigators and other providers often do the same. Indeed, being involved in a patient’s positive transformation can result in vicarious transformation for the provider, who can derive a sense of meaning, growth, and purpose from patients’ empowerment.
Dr Parekh outlined for attendees the ABCs of vicarious resilience:
- A – Acceptance that vicarious trauma is an occupational hazard and a normal response, as well as that overcoming it is a process
- B – Balance of work and leisure activities, as well as one’s caseload with various types of patients
- C – Connection with oneself and others, as well as with a sense of spirituality.
“It’s a process; it doesn’t happen overnight,” Dr Parekh said. “When we’re able to see our patients become more empowered, we become more empowered.”
When the Clock Is Ticking: The Importance of Fertility Preservation for Adolescent and Young Adult Patients with Cancer
For patients with cancer in their childbearing years, fertility preservation is a time-sensitive survivorship issue that must be addressed. Traditionally considered the responsibility of the oncologist, conversations around fertility preservation have become a duty with which the medical team as a whole is charged, thanks to 2018 guideline updates from the American Society of Clinical Oncology (ASCO).
“We want to try to have this conversation before any form of treatment is introduced into their body,” said Megan Solinger, MHS, MA, OPN-CG, Director of Patient Navigation and Adolescent and Young Adult (AYA) Patient Navigator at UMMC Ulman Foundation, Baltimore, MD.
Sharing insights on the importance of fertility preservation for AYA patients with cancer, she also discussed how to confront the issue to avoid a missed opportunity for patients.
“I always say fertility preservation is like an insurance policy for patients,” Ms Solinger said.
Despite the urgency of preserving fertility before treatment ensues, less than half of oncologists discuss the topic with patients, according to Ms Solinger. Faced with multiple barriers, oncologists and other healthcare providers—including navigators—often find themselves avoiding the topic, to the detriment of the patient. Some obstacles to such discussions are providers’ belief system surrounding fertility; assumptions about the patient’s interest in, or ability to afford, fertility preservation; lack of knowledge; focus on treatment and survivorship; and general discomfort with discussing it.
From the patients’ perspectives, barriers to preserving fertility include financial constraints; focusing on treatment and survival; lack of time to pursue fertility preservation before the start of treatment; lack of knowledge; childbearing being a distant consideration; no current desire to have children; and uncertainty about who to approach with their concerns about fertility.
“That may be a distant thought,” Ms Solinger said, adding that some AYA patients may feel that they do not want children but such a decision may change over time. “We as people evolve, we grow, we have experiences, and we may change our minds about things.”
Preparing for conversations about fertility preservation involves becoming educated on available options, the processes involved, and their costs, as well as resources available to patients, according to Ms Solinger. As part of this preparation, navigators and other providers should familiarize themselves with fertility clinics within their health system or elsewhere, with which they can form partnerships and referral mechanisms to expedite the process for patients.
“Once they finish treatment, they can get their fertility checked by a reproductive endocrinologist,” she said. “This is something I recommend.”
When it comes time for “the talk,” it is important to first gauge the level of knowledge and understanding on the part of the patient and family members, Ms Solinger said. From there, the provider should explain the process of fertility preservation, along with what to expect, and available options. The patient and family members should emerge from the discussion feeling empowered to begin taking action, if desired.
“I mention to people that there are family-building options besides having a biological child,” she said. “It is a tough conversation to have but there are things that give people hope, no matter what the situation looks like.”
Key things to remember when having fertility preservations discussions include:
- Ask patients if anyone has discussed the topic with them
- Find out who the patient would like in the room for the discussion
- Speak in terms, and at a level, the patient understands
- Be patient, understanding, and thorough
- Repeat what has been discussed; if possible, use the teach-back method
- Provide informational handouts
- Give the patient and their family time to discuss among themselves
- Check repeatedly with the patient about their final decision
- Document all information in the patient record
- Go in prepared.
Take Charge (letstakecharge.org) is a robust resource tailored to the needs of young patients with cancer, as well as their caregivers and healthcare providers. In addition, the Moffitt Cancer Center offers a free, online 8-week program called ECHO (Enriching Communication Skills for Health Professionals in Oncofertility), which equips clinicians with the necessary skills to help patients traverse the terrain of fertility preservation.
“It is one of the best training programs I have found out there,” Ms Solinger said.
With costs for fertility preservation ranging in the thousands and third-party options reaching into the tens of thousands, it is fortunate that resources exist to offset the financial burden. Organizations including Livestrong, Team Maggie for a Cure, and Verna’s Purse offer financial assistance, and local nonprofits may offer smaller grants. Pharmaceutical companies and fertility clinics may donate medications, and oncofertility consultations may be offered free of charge. In addition, providers should encourage patients to check with their insurance companies regarding coverage for iatrogenic infertility, Ms Solinger said.
Institutions should enact a fertility preservation policy that applies to any type of iatrogenic infertility. A requirement of Centers of Excellence, such a policy should be easy to follow and access.
Amid the exciting milestones that punctuate one’s 17th year, including becoming a licensed driver, attending prom, and preparing to graduate high school and move into adulthood, Bret Miller had a nagging concern—a small, hard lump under his right nipple.
During multiple physicals around that time, his worry was assuaged. The doctor told him the lump was a mere calcium buildup, a result of puberty that would go away over time. When 7 years had passed and the lump was still there, Mr Miller asked his doctor to check it out. This time, the doctor recommended he have a sonogram done. After having the imaging done at a women’s clinic, doctors there recommended he have a mammogram that same day.
“There I am, walking down the hall in the pink gown to go get the mammogram,” Mr Miller, a Kansas City, KS, native recalled.
Shortly thereafter, doctors removed the lump, still believing it was a calcium deposit. It was the day after, April 28, 2010, when the doctor called to say preliminary reports showed breast cancer, and that someone would get back to Mr Miller in 3 to 5 days, when they had the chance to fully review the report.
“And that was pretty much it—no ‘Hey, you should really come in, we need to discuss these results,’ ‘Are you sitting down,’ or anything of a bedside manner to really help out, so I was really shell shocked, like a bomb,” he recalled.
At work at the time, Mr Miller called his father, Bob, to share the news. Because he was unable to discuss it at length, he asked that his diagnosis not be shared with his mother, Peggy, just yet. Five minutes later, she called, understandably worried and upset. The next day, thanks to Peggy’s advocacy, they were back at the doctor’s office, discussing the results.
With the help of his parents, Mr Miller was set up with those he refers to as his “angels.” Nurse navigator Mary Williams was one of them.
“She helped out tremendously,” he said. “They helped get my case into the top hands of the local doctors and that ended up helping me to get the best treatment.”
A second opinion came from a surgeon with whom Mr Miller felt comfortable and confident. It was this surgeon who ended up performing a single mastectomy on him on May 18, 2010.
“He said that he saw something in me, that if I was willing to share my story, he said he saw me as the face of male breast cancer, out there helping other men be comfortable with the diagnosis,” Mr Miller recalled, saying the doctor added that all 12 of his previous male breast cancer patients had quietly gone about their lives after treatment, choosing not to speak out.
The surgery was a success, and that moment represented a turning point for Mr Miller. He knew he could not be silent about the disease.
“This is bigger than me and a diagnosis. This is something that really needs to be talked about,” he asserted. “This is not a women’s disease. This is a people’s disease.”
With that in mind, he started the Bret Miller 1T Foundation only a day after his mastectomy, with the goal of raising awareness of male breast cancer among high school and college students. Four years later, he connected with fellow advocate Cheri Ambrose, and they teamed up as co-founders of the Male Breast Cancer Coalition.
“We are a very large, global resource support group for men, just to let them know that they are not alone when they hear the words, ‘You have breast cancer,’” Mr Miller said, adding that estimates say approximately 2600 US men will hear those words this year, but he and other advocates believe that number is actually higher. “We just want to make sure men are included in research, in trials, and in the terminology.”
He recalled the hurdles he had to overcome as a man with breast cancer, in addition to the significant burdens that already come with the disease.
“There were times that I was addressed as a female in paperwork, and having to go through women’s clinics for everything, which was also very off-putting and emasculating,” Mr Miller said, adding that clinics could help by scheduling male patients at the beginning or end of the day. “We always say we’re just trying to put a splash of blue in a sea of pink.”
Genetic testing determined he did not have a BRCA mutation, and the Oncotype DX® assay revealed he had a 22% risk for recurrence over the next decade. Being told 4 rounds of chemotherapy would reduce that risk by up to 10%, he was all for it. After a stint with tamoxifen had Mr Miller experiencing hormonal side effects, he switched to anastrozole.
“I did that for 5 years, and I’ve been free of cancer ever since,” he said, adding, “Be your own best advocate. If you feel something, say something. Know your doctor. Get second, third, fourth opinions, whatever it is until you feel comfortable.”
For more information, visit malebreastcancercoalition.org.














